Granulomatous polyangiitis (GPA), formerly known as Wegener’s granulomatosis, is a rare autoimmune disease characterized by inflammation of the blood vessels (vasculitis) that usually affects small and medium-sized blood vessels. It usually affects the nose, nose, lungs, and kidneys, but can also affect other organs. While the exact cause of. (Know more about Granulomatosis with Polyangiitis, Symptoms, Diagnosis and Treatment)
GPA is unknown, it is thought to involve a combination of genetics and environment. Antibiotics are believed to cause inflammation and nerve damage.
The symptoms of GPA vary depending on the body involved, but generally include:
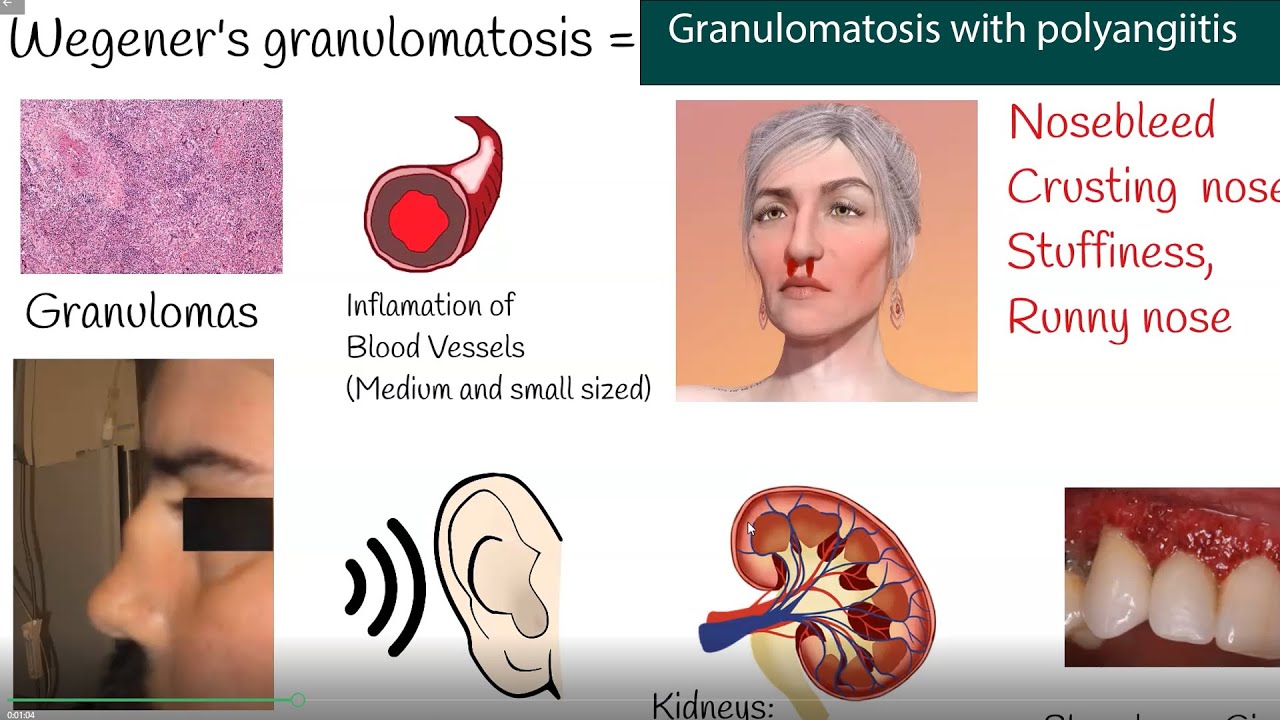
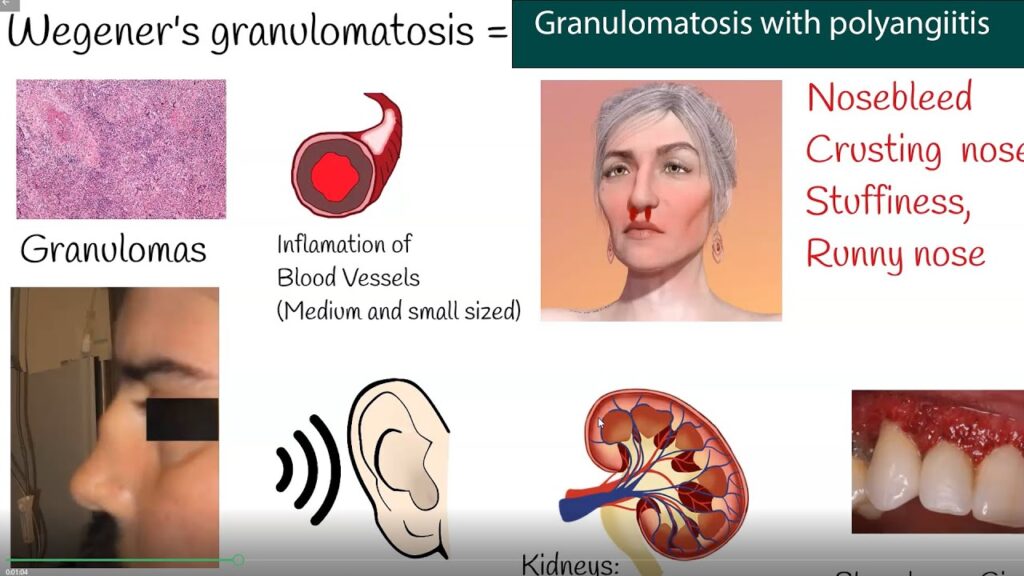
Upper respiratory tract symptoms: Acute sinusitis, nasal congestion, epistaxis, and crusting.
Pulmonary symptoms: cough, shortness of breath, chest pain, coughing up blood.
Renal symptoms: hematuria (blood in the urine), proteinuria (high protein in the urine) and kidney failure.
Joint and muscle pain: Arthralgia (arthralgia) and myalgia (muscle pain).
Skin Diseases: Red bumps, bumps, or sores on the skin. If
GPA is left untreated, it can lead to serious complications such as kidney failure, lung disease, and damage to other organs.
Therefore, diagnosis at early stage and after treatment is very important.
The diagnosis of GPA requires a combination of clinical evaluation, laboratory tests, imaging studies, and sometimes a biopsy from the affected tissue. Blood tests can show high levels of certain antibodies, such as antineutrophil cytoplasmic antibodies (ANCA), which are often associated with GPA.
The mainstay of GPA treatment includes the use of anti-inflammatory drugs to prevent organ damage and control inflammation. Corticosteroids such as prednisone are often used initially to promote remission.
Other anti-inflammatory drugs such as cyclophosphamide or rituximab may be added to achieve remission, followed by treatment with less effective drugs such as methotrexate or azathioprine.
Regular doctor visits are necessary to monitor disease activity, check for side effects of medications and treat as needed.
Note that the information provided here is for general information purposes only and you should consult a physician for specific advice and guidance regarding your situation. Know more about Granulomatosis with Polyangiitis, Symptoms, Diagnosis and Treatment.
Granulomatosis with Polyangiitis Symptoms
Granulomatous polyangiitis (GPA), formerly known as Wegener’s granulomatosis, is a rare autoimmune disease that often affects blood vessels in many parts of the body, including the nose, sinuses, lungs, and kidneys. This disease is caused by inflammation and the formation of granulomas, which are clumps of inflamed cells.
The symptoms of granulomatous polyangiitis vary from person to person, and the severity of the disease can range from mild to severe. Here are some symptoms associated with GPA:
Upper respiratory tract symptoms: GPA often affects the upper respiratory tract, causing symptoms such as sinusitis, nasal congestion, bleeding, nose and ear. Some people may also have pain or tenderness in the nose or face.
Pulmonary symptoms: Pulmonary involvement is common in GPA. It causes symptoms such as coughing, shortness of breath, chest pain and coughing up blood (hemoptysis). Inflammation in the lungs can lead to complications such as pneumonia or lung nodules.
Kidney problems: GPA can affect the kidneys, causing glomerulonephritis. Symptoms may include blood in the urine (hematuria), protein in the urine (proteinuria), low urine output, high blood pressure, and swelling in the legs or other parts of the body due to water retention.
Joint pain and muscle pain: Some people with GPA may experience joint pain, muscle pain, or arthritis-like symptoms. The most common joints include the knees, ankles, and wrists.
Skin symptoms: Skin rashes or rashes may occur in some cases of GPA. Pain, tenderness, or soreness may occur in these areas, especially in areas exposed to sunlight or stress.
Eye problems: Eye problems can cause redness, pain and blurred vision.
In severe cases, it can lead to scleritis, uveitis or other serious eye problems.
Legal Symptoms: People with GPA may experience symptoms such as fatigue, weight loss, fever, night sweats, and a feeling of weakness.
It is important to note that these symptoms are not specific to GPA and may occur in other conditions. If you have persistent symptoms or concerns, it is important to consult a doctor to find out the truth and correct it.
Granulomatosis with Polyangiitis Diagnosis
Granulomatous polyangiitis (GPA), formerly known as Wegener’s granulomatosis, is a rare autoimmune disease that affects blood vessels, causing inflammation and damage to many organs. Diagnosis of GPA usually includes a clinical examination, laboratory tests, scientific testing, and sometimes a biopsy. Here are the simple steps to check for GPA:
Medical history and physical exam: Your doctor will review your medical history, including the symptoms you’re experiencing, and perform a thorough physical exam to monitor for signs of GPA, such as sinus or breathing. problems. problems, joint pain, skin disease or kidney abnormalities.
Blood tests: Several blood tests can be done to assess your general health and check for certain markers related to GPA. These tests may include:
Complete blood count (CBC): To measure the level of red blood cells, white blood cells, and platelets.
Erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP): measures inflammation in the body.
Antineutrophil Cytoplasmic Antibodies (ANCA): ANCA testing is often important for diagnosing GPA. There are two common types of ANCA tests: cytoplasmic ANCA (c-ANCA) and perinuclear ANCA (p-ANCA). A positive c-ANCA test is a good indicator of GPA, but not all GPA patients have a positive ANCA result.
Kidney function test: To measure how well your kidneys are working.
Diagnostic Imaging: Imaging tests help identify disease-related conditions and detect abnormalities. Commonly used imaging techniques include:
Chest X-ray: to examine the lungs for nodules, cavities, or other signs of abnormalities.
Computed Tomography (CT) Scan: A more detailed scan that provides detailed images of many organs, such as the lungs, sinuses, or kidneys.
Magnetic Resonance Imaging (MRI): It is particularly useful in evaluating diseases that affect certain areas such as the brain or spinal cord.
Biopsy: In some cases, tissue biopsy is required to confirm the diagnosis of GPA.
A small sample of tissue, such as the lungs, sinuses, or kidneys, is collected and examined under a microscope to look for characteristic granulomas and vasculitis.
It’s worth noting that diagnosing GPA can be difficult, as symptoms can be similar to other conditions. Therefore, a multidisciplinary approach is required for accurate diagnosis, often consisting of rheumatologists, pulmonologists, nephrologists and other specialists. If you think you may have GPA, it’s important to consult a doctor who can evaluate your symptoms and do the appropriate tests.
Granulomatosis with Polyangiitis Treatment
Granulomatous polyangiitis (GPA), formerly known as Wegener’s granulomatosis, is a rare autoimmune disease that often affects blood vessels in many parts of the body, causing pain and tissue damage. Treatment for granulomatous polyangiitis usually includes a combination of medications to prevent infection and control symptoms. The main treatments are:
Glucocorticoids (steroids): High-dose corticosteroids (such as prednisone) are usually the first line of treatment for GPA. They help reduce inflammation and strengthen the body’s immune system. At first, higher doses will be prescribed, with the dose being gradually reduced as the condition improves.
Antibiotics: Antibiotics are used to control the infection and prevent its recurrence. Commonly used anti-inflammatory drugs include:
A) Methotrexate: Often used as a steroid sparing drug to help reduce the dose and side effects of corticosteroids.
B) Azathioprine: This drug is usually used to treat disease in remission.
mycophenolate mofetil: It is another antibiotic that can be used in treatment.
C) Rituximab: This is a monoclonal antibody that targets B cells involved in the autoimmune response.
Plasma exchange (plasma exchange): Sometimes plasma exchange can be used to remove inflammatory antibodies from the blood. This procedure is usually reserved for serious diseases such as kidney disease.
Support Services: Depending on the extent of the physical involvement, additional medical care may be required. For example, if GPA is affecting the kidneys, medication should be used to control blood pressure and maintain kidney function.
It is important to remember that the treatment plan will vary according to the severity of the disease, its physical effects, and the patient’s condition. Medical decisions should be made in consultation with a rheumatologist or physician familiar with the GPA. Regular monitoring and evaluation are important to assess response to treatment and adjust dose as needed.